Advancements in Brain-Machine Interfaces: Exploring Predictive Implants and Ultra-Low Power Chips
The world's first-in-human clinical trial using invasive intelligent brain devices has shown significant success in predicting specific neuronal events. These devices can forecast brain activity before specific outcomes, offering unprecedented applications in enhancing patients' quality of life. The use of predictive brain implants, designed to provide real-time advice on how to respond to forecasted neuronal events, raises profound ethical concerns regarding patient autonomy.
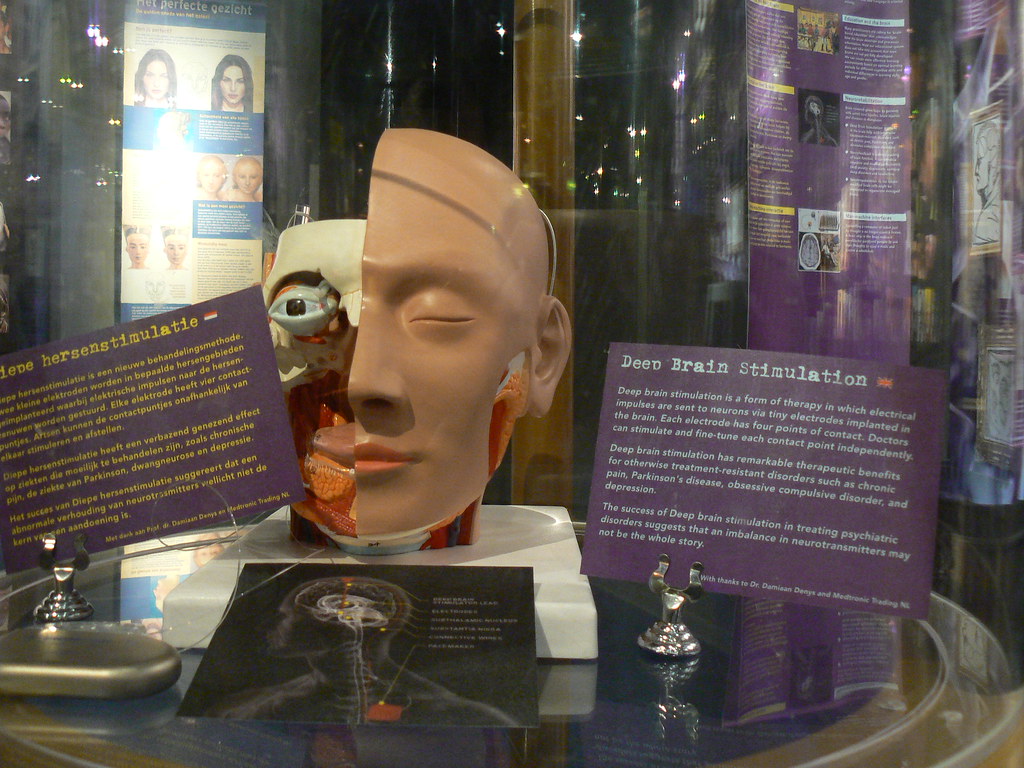
Implantable brain technologies are increasingly being adopted globally, with over 100,000 patients treated using invasive methods like deep brain stimulation (DBS). Recent studies suggest that these devices are beneficial in the early stages of neurological diseases, prompting a shift from late-stage interventions to early implantation. This shift could revolutionize treatment methodologies, challenging traditional pharmaceutical approaches.
The predictive functionalities of these devices involve advising patients ahead of time about oncoming symptoms or automatically administering therapeutic responses. For instance, successful trials have demonstrated the ability of these devices to predict epileptic seizures, allowing individuals to prepare and potentially prevent these episodes. Approximately 1% of the global population suffers from epilepsy, with many cases inadequately controlled by existing treatments.
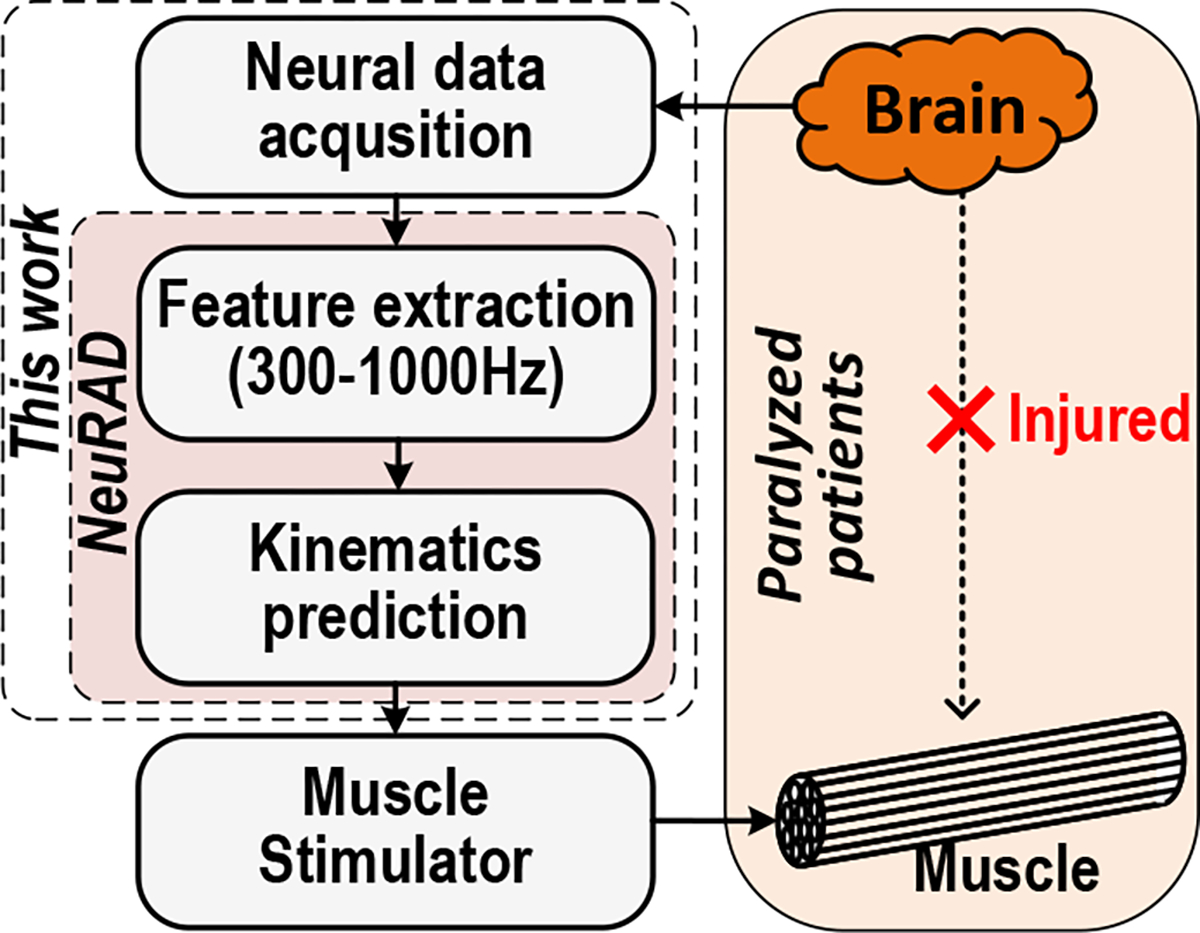
Image courtesy of PMC
Ethical Concerns of Predictive Brain Devices
The introduction of predictive brain implants carries ethical dilemmas that need addressing. The invasive nature of these devices, combined with their ability to monitor brain activity continuously, raises questions about patient autonomy. Key ethical inquiries include the effects of ongoing monitoring on a patient’s autonomy and the risks associated with overreliance on these technologies.
Current medical literature often emphasizes physical safety concerns, such as device-related adverse events, but less attention is given to postoperative psychological impacts. A phenomenon known as the Burden of Normality Syndrome raises questions about whether successfully treated individuals may struggle with adjusting to a "normal" state. Understanding these risks is vital, as they can affect a patient’s self-determination and overall mental health.
Patient Experiences with Predictive Devices
A pilot study involving a patient implanted with an advisory brain device for epilepsy management illustrated the complex interplay between technology and autonomy. The patient reported feeling more in control of his life, empowered by the device’s ability to predict seizures. Such experiences underscore the nuanced relationship between predictive technologies and a patient’s sense of autonomy.
Patients expressed feelings of increased independence due to the device monitoring their brain activity, which alleviated the unpredictability of seizures. This suggests that while predictive functionalities enhance control, they may simultaneously introduce new layers of dependency that could complicate the patient's autonomy.
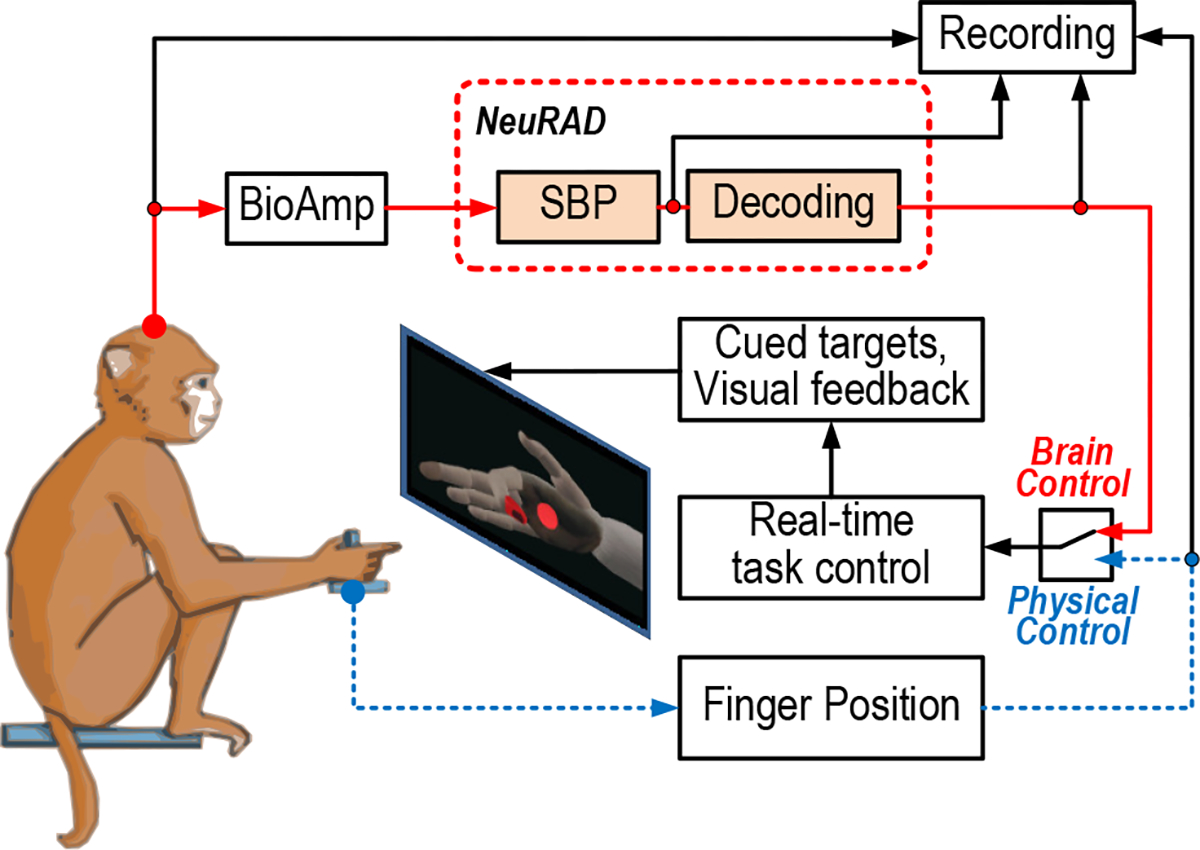
Image courtesy of PMC
The Future of Brain-Machine Interfaces
Recent advancements in brain-machine interfaces (BMIs) focus on creating low-power, implantable devices capable of real-time decoding of neural signals. A new application-specific integrated circuit (ASIC) called NeuRAD has demonstrated significant power efficiency, consuming less than 600 μW while predicting finger movements in nonhuman primates. This breakthrough could pave the way for portable neural prostheses, which could restore motor functions for individuals with spinal cord injuries.
The NeuRAD ASIC incorporates hardware accelerators for efficient feature extraction and decoding, marking a significant advancement in minimizing power consumption for implantable devices. Such developments are crucial for enhancing the usability of brain implants in real-world scenarios, ensuring they can operate safely and effectively in various environments.
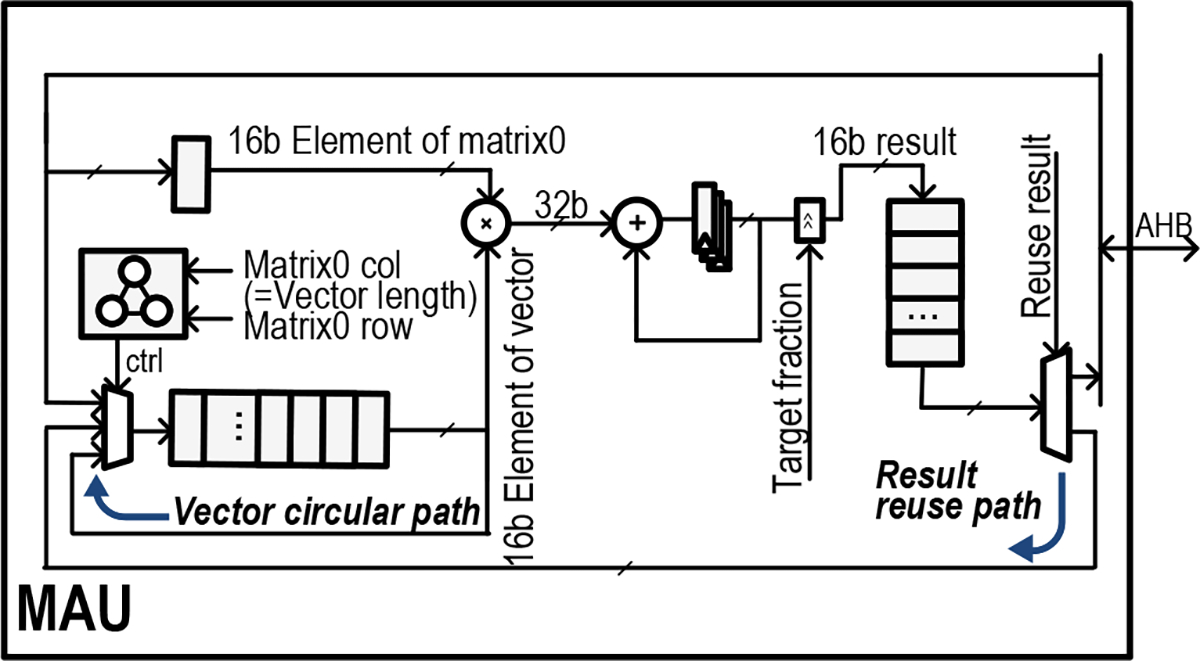
Image courtesy of PMC
Innovations like Purdue University's tiny, ultra-low power chips are also contributing to the understanding of neurological conditions. These chips, which can wirelessly transmit brain signals without external batteries, represent a leap toward practical neuroprosthetics that could one day facilitate nerve injury repair and long-term brain health monitoring.